This is a major area of modern knee surgery, where the focus is on restoring normality to the knee.
First published in 2016, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
Surgical cartilage repair for knee osteoarthritis
This is a major area of modern knee surgery, where the focus is on restoring normality to the knee.
First published in 2016, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
This is a procedure to flatten the softened and roughened joint cartilage at the early stages of breakdown, to clear away any damaged bits and stop and enzyme release which might further the damage. The cartilage damage at this stage has not gone quite through to the bone and the defect can heal over more or less.
In abrasion arthroplasty the surgeon uses a rotating burr to rub away damaged bits of joint cartilage right until there is bleeding of the underlying bone, in the hope that progenitor cells from the bone marrow will migrate into the area and turn themselves into a type of cartilage called 'fibrocartilage'.
Issues with abrasion arthroplasty include:

Microfracture is a related marrow stimulation technique that avoids a burr but instead a sharp pick-like instrument is gently knocked through the damaged cartilage surface and through the plate that separates it from the bone, to create a number of small pucture wounds going into the bone marrow. This stimulates bleeding, and blood enters the hole and clots there, bring with it the progenitor cells that can create fibrocartilage and cover the defect. After microfracture the patient needs to use crutches for quite a number of weeks to avoid damaging the new tissue layer.
Nanofracture is a newer procedure that makes smaller and less traumatic holes.
Reviewing subchondral cartilage surgery: considerations for standardised and outcome predictable cartilage remodelling.Benthien JP and Behrens P. Int Orthop. 2013 Nov; 37(11): 2139–2145.
This is a technique for medium sized areas of discrete damage. The surgeon uses an instrument a bit like an apple-corer to core out a circle of damaged cartilage and replaces it with a piece of normal cartilage from a less important part of the same knee. The principle here is that this grows to cover the edges of the core using proper cartilage cells and not the weaker fibrocartialge cells.
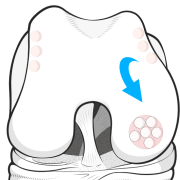
Mosaicplasty is used for even larger but discrete areas of damage. The damage is debrided and the recipient bed prepared ready to be packed with a number of small bone/cartilage cores harvested from less important parts of the knee, such as along the non-weight-bearing edge of the femoral condyle. This technique results in the damaged area being repaired with true cartilage mixed with fibrocartilage, which is stronger than fibrocartilage alone.
Knee donor-site morbidity after mosaicplasty – a systematic review.Andrade R, Vasta S, Pereira R, Pereira H, Papalia R, Karahan M, Oliveira JM, Reis RL and Espregueira-Mendes J. J Exp Orthop. 2016 Dec; 3: 31.
This technique is used in some areas but has not generally become popular. Normal cartilage is taken and ground up into a paste and pasted back into the damaged area.
Large areas of damage do not mean you have to give up the ghost on this cartilage regeneration thing. The surgeon can take a little bit of normal cartilage and send it to a lab to be cultured and then in a second operation the cells are injected into the damaged area which has been prepared by a flap of fibrous material from over the bone being sewed over the damaged area to retain the cells.
The AMIC procedure is actually a combination of two steps. The first is preparation of the bed of an arthritic defect with a marrow stimulation pick (microfracture) and then overlaying the area with a collagen scaffold. Blood and mesenchymal stem cells can pass into the area from underlying bone marrow, and form a clot, which is then stabilised and held in place by the collagen membrane until fibrocartilage forms. A variation is NAMIC, where nanofracture is used instead of microfracture.
Enhanced microfracture techniques in cartilage knee surgery: Fact or fiction?.Bark S, Piontek T, Behrens P, Mkalaluh S, Varoga D and Gille J. World J Orthop. 2014 Sep 18; 5(4): 444–449.