A failure to introduce the arthroscopic camera and instrumentation properly may leave the surgeon totally disorientated.
First published by knee surgeon Angus Strover in 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
A system of examination from the standard portals
A failure to introduce the arthroscopic camera and instrumentation properly may leave the surgeon totally disorientated.
First published by knee surgeon Angus Strover in 2008, and reviewed August 2023 by Dr Sheila Strover (Clinical Editor)
If it is placed too close to the patellar tendon, one might lose one's way in the body of the fat pad, which lies just under the tendon. All the surgeon will see is a bright yellow colour, and not the shiny white surfaces you are starting to recognise. Removing the obstructing fat can be traumatic, and the patient can be left with a scarred and painful fat pad, and even the serious complication of 'infrapatellar contracture syndrome'.
If the first portal is too low, then it will be below the meniscus and tibial plateau, and it will be difficult to navigate the arthroscope to the other side.
Continue to the next bit to see the kind of mess an amateur finds himself in .... Click the arrow under the play to start the video. If you cannot get the player to work don't worry - I will also show some still images to demonstrate the principle. Please note that there is no sound.
This is an example of how NOT to do an arthroscopy. The surgeon is lost in this knee - he is desperately hunting around to find a landmark he can recognise.
Here are a couple of stills from the video, which just showed a swirling mass of undefinable tissue -


The view should be crystal clear. Failure to see the anatomy clearly may be because -
I mentioned before the possibility of using a wide-bore inflow cannula to ensure optimal pressure using a pressure pump. Here is a picture of this cannula.
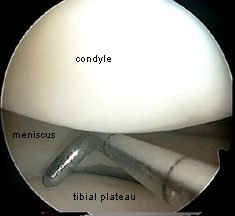
Now I am going to take you through a more expert diagnostic arthroscopy, step by step. If you cannot view the videos, there will be an opportunity each time to see stills. I am going to show first video again. This time you will appreciate how clear the image is. Note:
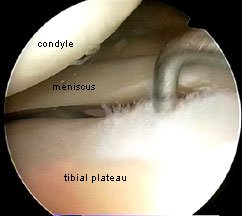
Click the video arrow button to start the video... See how after fully examining the meniscus and joint surfaces on the medial side, the surgeon swings the probe over into the notch to explore the cruciate ligaments ...

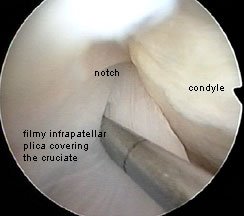
In this next video the probe is in the notch. The surgeon is trying to examine the cruciate ligaments. At first glance looks as if they are fine. But when the surgeon tries to pull on them with the probe, he discovers that what he is seeing is not the cruciates at all - but a filmy infra-patellar plica masquerading as a cruciate! Such plicae are not always present. After 'hoovering' away the plica, the real cruciate is revealed below. Now pulling on it tests its true integrity.
From this position, still with the scope in the original portal, the surgeon can slip the probe round the back of the cruciate and test the posterior horn of the lateral meniscus, the body of the meniscus and the joint surfaces as before.


Now a surgeon, and especially an arthroscopic surgeon, has to train himself to be ambidextrous.
If he finds it hard to see a part of anatomy, he needs to remove the instruments and swop their positions around, coming in from the other side, or maybe even a third or fourth portal. This can cause the novice a problem, as it is often hard to locate the portal again, as the tissues are in layers and the gap can appear invisible. I teach the use of what I call a 'switching stick', to allow a quick and easy changeover, without losing the portal. Failure to do this can result in long delays in the operating room, and the surgeon may need to start all over making the portal again!
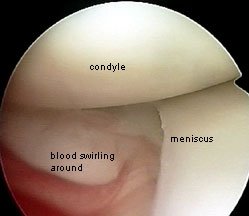
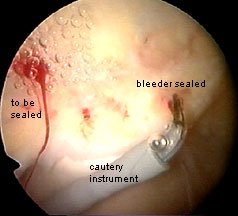
And while I am talking about problems, I just want to mention again the issue of bleeding. It is quite easy to see when you have cut a bleeder. I make sure that any bleeders are cauterised.