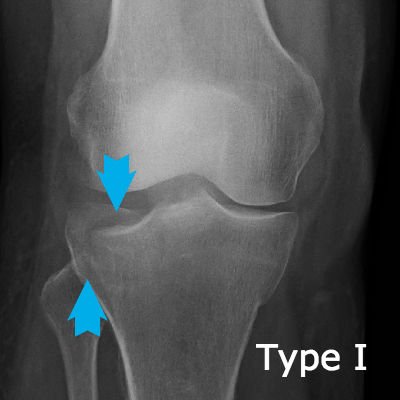
Tibial plateau fractures are very significant because the break goes through the joint line and upsets the dynamics of the joint. This X-ray shows a Schatzker Type I fracture.
A tibial plateau fracture is a bone break through the flat top end of the shin bone (tibia). Page updated January 2024 by Dr Sheila Strover (Clinical Editor)
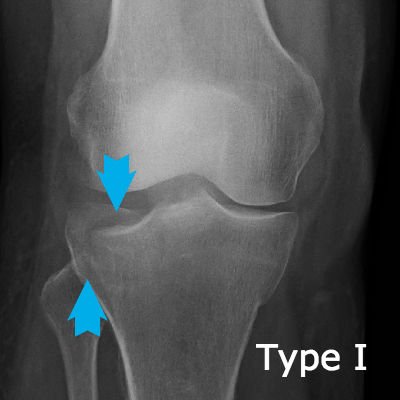
Tibial plateau fractures are very significant because the break goes through the joint line and upsets the dynamics of the joint. This X-ray shows a Schatzker Type I fracture.
The tibial plateau is an important area because it is where the two menisci are seated and the two cruciate ligaments are tethered, both of which function as knee stabilisers.
Fractures or bone breaks of the tibial plateau not only have the potential to upset the delicate mechanics of the knee, but they are also frequently missed by the emergency team despite the patient complaining of severe pain in the knee following an injury.
One needs X-rays in two different planes to be able to see the often subtle outline of the fractured area. Also, the bone may not necessarily break off, but may be crushed and the fragment depressed, and it needs an experienced eye to appreciate this on X-ray.

Tibial plateau fractures are graded according to the Schatzker classification, so that anyone reviewing the patient's notes have an idea immediately of the severity of the problem.
Tibial plateau fractures can be difficult to manage and cause problems with rehabilitation. Key issues include:
Assessing the degree of emergency - the injury may include damage to soft tissue structures as well as bone, including the menisci, nerves, blood vessels and ligaments. Some cases can be managed without surgery if the damage is not too severe. Very often, however, the initial management requires open surgery, and if there is vascular damage, including compartment syndrome, then immediate emergency surgery may be essential.
Restoring the anatomy - once attention has moved on from the immediate emergency, then the surgeon will attempt to evaluate the damage to the ligaments, especially the cruciate ligaments, and the degree to which any displacement of bone fragments is contributing to the functional damage. A CT scan may be called for so that the damage can be assessed in three dimensions, and the patient's bony injuries classified with the Schatzker classification for future reference. If there is no immediate emergency, blood in the joint (haemarthrosis) may be drained, and the limb put into a hinged brace until any surgery can be planned. Surgery might be undertaken in stages, trying to optimally align and fix in place the fractured pieces and restore ligament function.
Avoiding arthrofibrosis - in severe injuries like this, which may involve prologed periods of immobiisation and several surgeries, there is always a risk of residual stiffness from arthrofibrosis, and as much soft tissue mobility as is possible will become a focus as the bones unite.
Avoiding arthritis - long-term follow up will be necessary as there may be a strong possibility of future arthritis.
A physiotherapist ends up a patient after a nasty ski injury.
Patients discuss regaining range of motion after tibial plateau fracture.
Patients talk about extension lag after tibial plateau fracture, and how to improve things with physiotherapy.
A patient's own story after fracturing the tibial plateau in a ski accident.
A discussion about managing stiffness after TPF.
Quote:
Citation: Malik S, Herron T, Mabrouk A, et al. Tibial Plateau Fractures [Updated 2023 Apr 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470593/
Quote:
Citation: Ebrahimzadeh MH, Birjandinejad A, Moradi A, Fathi Choghadeh M, Rezazadeh J, Omidi-Kashani F. Clinical instability of the knee and functional differences following tibial plateau fractures versus distal femoral fractures. Trauma Mon. 2015 Feb;20(1):e21635. doi: 10.5812/traumamon.21635. Epub 2015 Feb 2. PMID: 25825697; PMCID: PMC4362032.